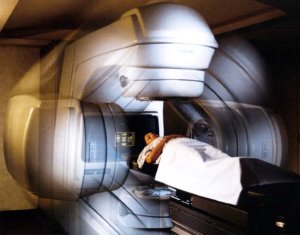
Image Guided Radiation Therapy can locate prostate cancer in real time, sparing the nearby structures during treatment. IGRT provides us with the ability to see what we’re treating every day and adapt your treatment as needed for the best possible outcomes.
Dr. Arun Puranik at Image Guided Radiation Therapy offers consultations to discuss your condition and whether radiation therapy best suits your needs. We encourage you to contact the office to schedule a consultation. The consultation provides you the opportunity to sit and speak with Dr. Puranik and openly discuss your questions and treatment plan.
Radiation therapy can be used to safely and effectively treat these types of cancers. If you have questions about a specific treatment, please contact our office for more information. We offer consultations to discuss your condition and treatment options that may work for you. Know that you are not alone in the process. We’re here to help you fight cancer.
Prostate cancer basics
 With the exception of skin cancers, prostate cancer is the most common cancer in American men. The American Cancer Society estimates that 186,320 new cases of prostate cancer will be diagnosed in the U.S. this year, and that 28,660 American men will die of this disease in 2008.
With the exception of skin cancers, prostate cancer is the most common cancer in American men. The American Cancer Society estimates that 186,320 new cases of prostate cancer will be diagnosed in the U.S. this year, and that 28,660 American men will die of this disease in 2008.
One man in five will be diagnosed with prostate cancer during his lifetime, yet only one in 33 will die of this disease.
Cancer is the uncontrolled growth of abnormal cells. Prostate cancer begins inside your prostate and may grow to involve the entire gland. Most prostate cancers are adenocarcinomas, meaning they develop from glandular cells.
As the cancer grows, it may spread to tissues or organs near your prostate gland. Eventually, prostate cancer may spread to other parts of your body, especially lymph nodes and bones, in a process called metastasis.
Detection
The early detection and treatment of prostate cancer is still an inexact science, but we can still make some general statements and recommendations.
Cancers found by digital rectal exam (DRE) or prostate-specific antigen (PSA) testing are usually in an early stage, which means they’re smaller and less likely to have spread than cancers causing symptoms.
If you choose to have early detection testing, you should begin at age 50. But if you are in a high-risk group — for example, if you had a father or brother diagnosed at a young age, or if you’re African-American – you should start testing when you’re 45.
PSA
Prostate-specific antigen (PSA) is a substance made by the normal prostate gland. Most PSA is in your semen and normally only a small amount enters your blood.
Most men have levels under 4 nanograms (a nanogram is a billionth of a gram) per milliliter of blood. Men with PSA between 2.5 and 4 have a 20% to 25% chance of having cancer. If your level is above 4, but less than 10, you have about a 30% to 35% chance of having prostate cancer.
If it goes above 10, your chance of having prostate cancer is more than 67% and rises even more as your PSA level increases.
PSA levels estimate how likely you are to have prostate cancer, but the test does not give a conclusive answer. Accurately diagnosing prostate cancer can only be done by performing a biopsy, which involves removing a sample of prostate tissue for examination.
Digital Rectal Exam (DRE)
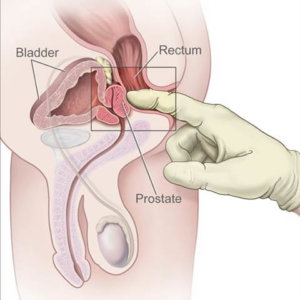 During this exam, your doctor inserts a gloved, lubricated finger into your rectum to feel for any irregular or abnormally firm area that could be a cancer. Your prostate is right in front of your rectum, and most prostate cancers begin in the part of the gland that is nearest your rectum and can be reached by a rectal exam.
During this exam, your doctor inserts a gloved, lubricated finger into your rectum to feel for any irregular or abnormally firm area that could be a cancer. Your prostate is right in front of your rectum, and most prostate cancers begin in the part of the gland that is nearest your rectum and can be reached by a rectal exam.
Prostate cancer is usually diagnosed with a blood test measuring the amount of prostate specific antigens (PSA) in the body. Symptoms can include:
- Changes in urinary flow: frequency, urgency, hesitancy
- Frequent night time urination
- Painful urination
- Blood in urine
Other conditions that may cause these symptoms include an enlarged prostate (also called benign prostatic hypertrophy or BPH) or infection.
Prostate Cancer Staging
 Staging is a standard way to describe how far your prostate cancer has spread within the prostate, to nearby tissues and to other organs. Knowing what stage your cancer is in is one of the most important factors in selecting treatment options, and a major factor in predicting your prognosis.
Staging is a standard way to describe how far your prostate cancer has spread within the prostate, to nearby tissues and to other organs. Knowing what stage your cancer is in is one of the most important factors in selecting treatment options, and a major factor in predicting your prognosis.
The most common staging system in the U.S. is the TNM System of the American Joint Committee on Cancer (AJCC). The TNM System describes the extent of primary tumor (T), the absence or presence of spread to nearby lymph nodes (N), and the absence or presence of spread (metastasis) to distant organs (M).
T Stages
T1 refers to a tumor not felt during a digital rectal exam, but whose cancer cells are found in a prostate biopsy or prostatectomy (removal of the prostate) specimen.
T2 means your doctor can feel the prostate cancer by DRE (digital rectal examination) and that your cancer is probably confined to the prostate gland.
T3 cancers have spread beyond the outer rim surrounding your prostate. They have reached the connective tissue next to the prostate or the seminal vesicles, but do not involve any other organs.
T4 means your cancer has spread to tissues next to your prostate other than the seminal vesicles. These tissues can include parts of your bladder, your rectum, muscles in your pelvis or the wall of your pelvis.
N and M Stages
N stages indicate the extent of spread to nearby lymph nodes in your pelvis, while M stages tell if your cancer has spread to distant lymph nodes, bones, or other organs such as the lungs, liver or brain.
Treatments
After prostate cancer has been diagnosed with a biopsy, you should discuss your treatment options with a radiation oncologist and a urologist. These options include radiation therapy, surgery, hormone therapy, “watchful waiting” and chemotherapy.
Radiation Therapy
 In this treatment, high energy x-rays kill your cancer cells. Radiation therapy is used to treat prostate cancer that is still confined to your prostate gland or has spread only to nearby tissue. If your disease is advanced, radiation may be employed to reduce the size of the tumor and provide relief from symptoms.
In this treatment, high energy x-rays kill your cancer cells. Radiation therapy is used to treat prostate cancer that is still confined to your prostate gland or has spread only to nearby tissue. If your disease is advanced, radiation may be employed to reduce the size of the tumor and provide relief from symptoms.
Radiation therapy treatment options for prostate cancer include:
- External beam radiation therapy
- Prostate brachytherapy
External Beam Radiation Therapy
External beam radiation therapy involves a series of daily outpatient treatments to accurately deliver radiation to your prostate. There are three main ways to provide external beam radiation therapy:
- 3-dimensional conformal radiation therapy combines multiple radiation treatment fields to deliver precise doses of radiation to your prostate. Tailoring each radiation beam to accurately focus on your tumor treats your prostate cancer while protecting nearby healthy tissue.
- Intensity modulated radiation therapy (IMRT), the latest advance in radiation delivery, improves on 3D conformal radiation therapy by modifying the intensity of the radiation in each beam. With iMRT, radiation doses to tissues in the target area can be adjusted more precisely, allowing a higher radiation dose to the prostate and reduced doses to nearby normal tissues. This means a greater chance for a cure with fewer side effects.
- Image Guided Intensity Modulated Radiation Therapy – normal structures and tumors can move between treatments due to differences in organ filling or movements while breathing. IGRT is radiation therapy, or often IMRT for deep seated tumors, guided by imaging equipment, such as CT, ultrasound or stereoscopic X-rays, taken in the treatment room just before the radiation treatment is delivered. All patients first undergo a CT scan as part of the planning process. The digital information from the CT scan is then transmitted to the treatment console to allow the therapists to compare the earlier image with the images taken just before treatment. This allows for better targeting of the cancer while avoiding nearby healthy tissue. In some cases, a tiny piece of material called a fiducial marker may be implanted near or in the tumor to help localize the tumor during IGRT.
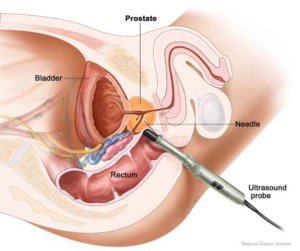
Prostate Brachytherapy
Also known as a seed implant, prostate brachytherapy is often done in the operating room. It delivers a very high dose of radiation to your tumor by inserting radioactive seeds directly into your prostate gland under ultrasound guidance while you are asleep.
Iodine or palladium is most commonly used. The seeds are about four millimeters long and less than a millimeter in diameter. Sometimes both prostate brachytherapy and external radiation may be used to combat your tumor.
Depending on the stage of your disease, you often have more than one treatment option to consider. Several factors should be taken into account when choosing these options, including potential benefits and risks.
Surgery
Surgery is often recommended to remove prostate tumors. Operations currently performed include:
- Radical prostatectomy or surgical removal of the prostate gland is used to treat cancer confined to your prostate. During the operation, the entire prostate gland and some tissue around it are removed.
- Transurethral resection involves removing part of your prostate with a tool that has a small wire loop on the end. The tool is inserted through your urethra up to your prostate gland. This approach is used for men who, because of age or illness, cannot have a radical prostatectomy to relieve urinary obstructions caused by the tumor.
- Cryosurgery involves inserting a metal probe directly into your tumor and freezing the tumor to destroy it.
Hormone Therapy
This treatment is often used if your prostate cancer has spread to other parts of your body or has come back after treatment. Hormone therapy seems to work better if it is started as early as possible after your cancer has reached an advanced stage.
The goal of hormone therapy is to lower the level of the male hormone testosterone, which is produced mainly in your testicles and causes prostate cancer cells to grow. Lowering testosterone can make your prostate cancer shrink or grow more slowly, but it does not cure your cancer.
Expectant Management (“Watchful Waiting”)
Another approach for you may be to “watch and wait.” While watching and waiting is not active treatment, it may be a good choice for you.
Your doctor may suggest a watch and wait approach if your cancer is small and contained within one area of the prostate, is expected to grow very slowly, and is not causing any symptoms. It may also be a good choice if you are elderly, frail or have other serious health problems. You may choose watchful waiting because you believe the side effects of aggressive treatments outweigh the benefits.
Because prostate cancer often spreads very slowly, many older men with the disease may never need any treatment. Active treatment can always be started later if the cancer begins to grow more quickly or causes problems.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. It is an option if your cancer has spread outside the prostate gland and if hormone therapy has failed.
Its goal is not to destroy all your cancer cells, but to slow tumor growth and reduce pain. The drugs flow through your bloodstream and kill cancer cells throughout the body. But they can also damage some normal cells. Your doctor must maintain a delicate balance of chemotherapy doses, making them strong enough to kill cancer cells while not harming healthy cells.
Side effects of chemotherapy vary but may include nausea and vomiting, hair loss and heart problems.
Frequently Asked Questions
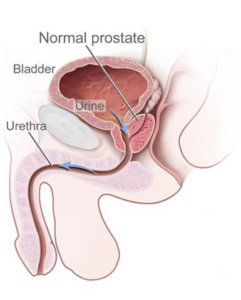
What is the prostate gland and what does it do?
The prostate gland is just below your bladder and in front of your rectum. It wraps around the tube called the urethra, which carries urine and semen out of the penis. The prostate makes a fluid that is part of the semen, the white fluid that contains sperm.
What is PSA?
PSA stands for prostate specific antigen. PSA is a chemical produced by normal and cancerous prostate cells. Other cells in your body produce virtually no PSA.
Normally, only a small amount of PSA gets into your bloodstream. But when your prostate is irritated, inflamed or damaged, such as in prostate cancer, PSA leaks into your bloodstream more easily, raising the level of PSA in your blood.
The normal range is 0 to 4. Once your baseline normal PSA has been obtained, your actual number becomes less important and your rate of change of PSA over time matters more.
What statistics do I need to know about prostate cancer?
Prostate cancer is the most common malignancy in American men other than skin cancer. The American Cancer Society (ACS) estimates that in 2008 about 186,320 new cases of prostate cancer will be diagnosed in the U.S. ACS also estimates that 28,660 American men will die of prostate cancer in 2008. More than 75% of prostate cancer is diagnosed in men over age 65.
What are the risk factors for prostate cancer?
The incidence of prostate cancer increases with age. The median age at diagnosis in Caucasian males is 71 (half are above that age, half are below). African-American men have the highest incidence of prostate cancer in the world. Heredity accounts for 5 to 10% of cases.
How do you screen for prostate cancer?
According to the American Cancer Society, men aged 50 or older should be offered a digital rectal exam (DRE) and a PSA blood test. But you should visit your doctor earlier to establish a baseline PSA level so you can monitor any changes.
Prostate specific antigen (PSA) is a valuable marker for prostate cancer, although an enlarged prostate or infection may also cause a rise in PSA. Normal range is 0-4, but a PSA above 3 in men younger than 60 could be abnormal. African-American men and men with a family history of prostate cancer should be tested beginning at an earlier age.
Links & Helpful Information
Zero – The Project to End Prostate Cancer
www.zerocancer.org
Prostate Cancer Foundation
www.prostatecancerfoundation.org
Us Too! International Prostate cancer Education and Support Network
www.ustoo.org
If you’d like to learn more regarding a diagnosis of prostate cancer or to schedule a consultation, contact IGRT today.